Victoria’s Ambulance Crisis: A Call for Urgent Reform
The current state of Victoria’s ambulance services has reached a critical juncture, as highlighted by alarming reports indicating that only one percent of the ambulance fleet was available to respond to emergency calls. This situation was sharply criticized by Sunrise host Nat Barr, who deemed the government’s handling of the crisis “ridiculous.”
Emergency Response Shortcomings
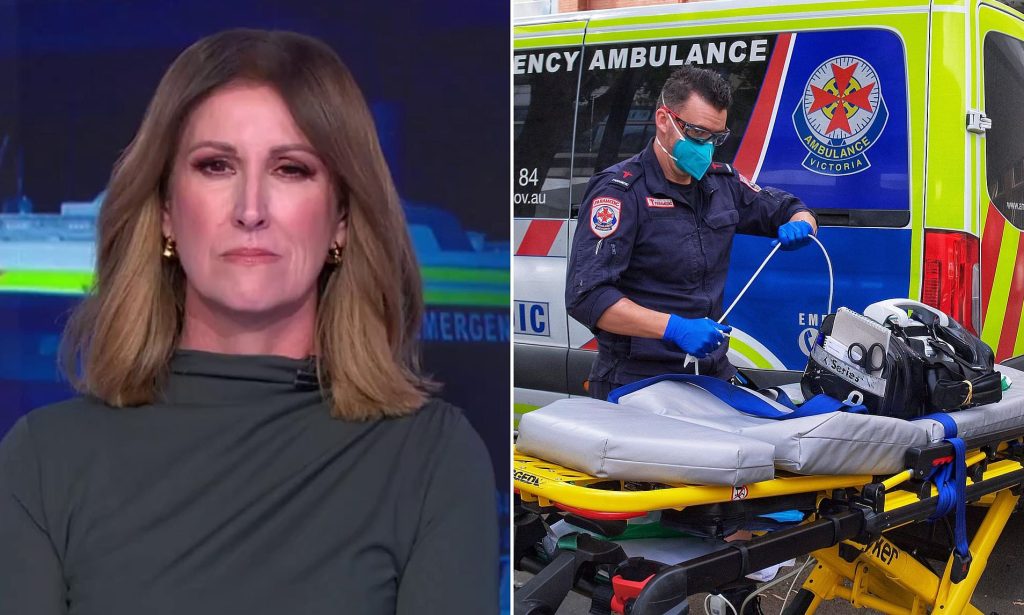
Recent incidents have shed light on the distressing reality faced by ambulance services in Victoria. On a particularly busy Monday night, over 50 individuals were left waiting for emergency medical assistance. Data revealed that more than 25 ambulance crews were unavailable due to staffing shortages, while at least 110 additional crews were stuck at hospitals, unable to return to the streets.
Paramedics found themselves in an untenable position, having to care for patients inside their vehicles while waiting for hospital beds to become available. This delay in transferring patients hindered their ability to respond to new emergencies, leaving the public vulnerable at a time when they needed help the most.
The Dire Situation According to Experts
Danny Hill, a representative from the Victorian Ambulance Union, detailed the severity of the crisis, noting that on that particular night, 22 advanced life support and eight mobile intensive care ambulances were not operational. The situation escalated to a point where approximately 100 crews were ramped at metropolitan hospitals, some waiting for as long as ten hours.
Hill emphasized that this left a mere one percent of the metropolitan ambulance fleet capable of responding to emergencies, an alarming statistic that underscores the strain on the system.
Public Outcry and Accountability
Nat Barr expressed her shock at the deterioration of Victoria’s public health sector, calling the situation an “absolute cluster” and urging for immediate intervention. She raised critical questions about the accountability of the ambulance service and the responsibilities of taxpayers who fund these essential services.
Hill reiterated the frustrations of paramedics, pointing out that they often find themselves diverted from emergency work to assist in hospital corridors, manage GP appointments, or address social issues. This misallocation of resources means that paramedics are frequently deployed to non-emergency situations, such as a recent call related to gaming addiction, which does not require their specialized skills.
Barr’s inquiries about the rationale behind sending paramedics to handle non-medical issues highlighted a systemic problem in the way emergency calls are triaged. Hill confirmed that while some patients might require assistance, they do not necessarily need the expertise of ambulance paramedics, indicating a need for better call management.
The Need for a Common-Sense Approach
Barr called for a sensible solution to the unacceptable conditions confronting Ambulance Victoria. Her assertion that “surely someone can fix this” echoed the sentiments of many who are frustrated by the ongoing crisis.
Further complicating the situation, leaked data revealed that more than ten major hospitals were experiencing wait times exceeding two hours by 8 PM, with some patients facing waits as long as ten hours.
Government Response and Public Health Challenges
In response to the escalating crisis, Premier Jacinta Allan attributed the surge in ambulance demand to the winter season. She noted that the community is facing the compounded effects of influenza, ongoing COVID-19 challenges, and other respiratory illnesses.
The urgency of the situation was underscored by the tragic incidents in June when two Victorians lost their lives while waiting for ambulances, including an elderly man from Blackburn who bled to death after a fall. Despite making two calls for an ambulance, he waited nearly five hours for assistance, while several crews were already ramped at a nearby hospital.
Conclusion
As the crisis unfolds, the need for immediate reforms in Victoria’s ambulance services has never been more pressing. The combination of staffing shortages, mismanagement of emergency calls, and overwhelming demands on hospitals has created a perfect storm that jeopardizes public health and safety. Stakeholders must come together to address these issues, ensuring that the ambulance service can fulfill its critical role in the community effectively and efficiently.